Knowledge Center

How Quality Child Care Translates into an Economic Development Tool
Columbus Mayor Skip Henderson didn't always see child care as an economic issue, but now the city is taking concrete steps to make quality child care more affordable and accessible for working families.
2026 ARPA Reporting Guide & FAQ
As the April 30, 2026 annual reporting deadline for the American Rescue Plan Act’s (ARPA) State and Local Fiscal Recovery Funds (SLFRF) approaches, many local governments have questions about the report and how to best prepare. This guide and frequently asked questions assists cities with the reporting process.
New Guides Help Cities Engage Young People in Civic Life
GeorgiaForward recently released two guides to help cities connect young people with civic life as part of the America250 celebration. In this Q&A, GeorgiaForward Managing Director Sadie Krawczyk talks about what's in the guides and how cities can put them to use.
Information Technology & Cybersecurity
Article
Top AI Investments Municipalities Should Budget for in 2026
February 24, 2026
Municipalities should budget for seven essential AI areas in 2026, along with an AI readiness assessment. These seven areas include licensing for AI productivity tools, AI enhanced cybersecurity, data analytics and governance, resident facing chatbots, AI integrations within existing systems, staff training, and pilot funding for future use cases.
Housing
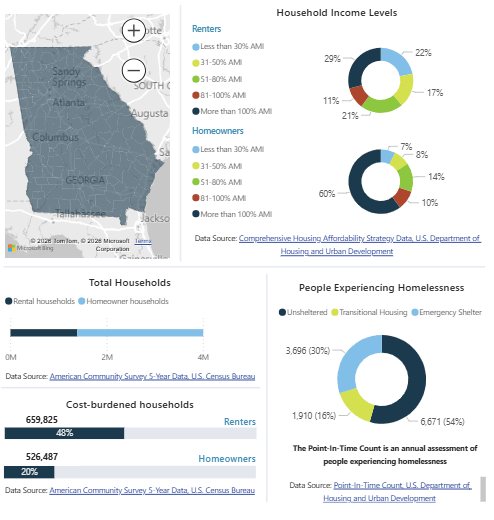
Data Dashboard
Housing Development Needs Dashboard
The DCA Housing Development Need Dashboard is an interactive platform to explore housing data on county- and on a regional-commission-level.
ARPA
American Rescue Plan Act
2026 ARPA Reporting Guide & FAQ
As the April 30, 2026 annual reporting deadline for the American Rescue Plan Act’s (ARPA) State and Local Fiscal Recovery Funds (SLFRF) approaches, many local governments have questions about the report and how to best prepare. This guide and frequently asked questions assists cities with the reporting process.

Children & Youth | Economic Development
Article
How Quality Child Care Translates into an Economic Development Tool
February 19, 2026
Columbus Mayor Skip Henderson didn't always see child care as an economic issue, but now the city is taking concrete steps to make quality child care more affordable and accessible for working families.
Taxation
Publication
Millage Rate Process Manual
This publication guides city staff through the millage rate setting process, from calculating the rollback rate to adopting the final millage and submitting required state forms.